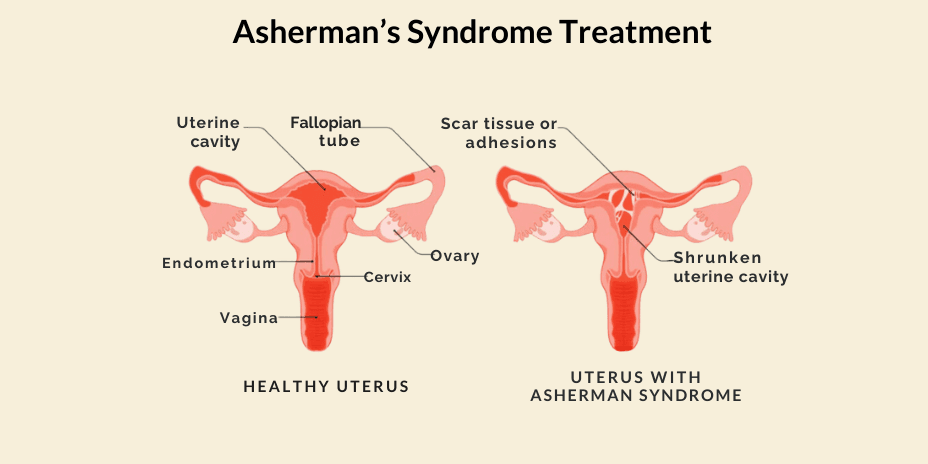
Asherman’s syndrome, also known as Intrauterine Synechiae(adhesions) and Uterine Synechiae, is a rare gynaecological condition in which the uterine cavity develops adhesions (scar tissue). An adhesion is nothing but a band of scar tissue that initially develops as part of the human body’s repair mechanism in response to any tissue disturbances, for instance, from previous surgeries. In most of the cases, the front & back walls of the uterus stick to each other. In other cases, adhesions develop only in a small portion of the uterus. The extent of adhesion helps to determine whether the case is mild or severe. Adhesions can be thick, thin, spotty in location or confluent.
CAUSES AND RISK FACTORS
In the majority of cases, Asherman’s syndrome occurs in women who have had procedures done associated with the uterus & pregnancy. In other cases, Asherman’s syndrome can be caused by infections involving the uterus or instrumentation before pregnancy.
Procedures of the uterus related to pregnancy
Dilation & Curettage or Dilation & Evaluation: Dilation is performed to widen the cervix so as to allow instruments into the uterus. Curettage is the procedure of scraping the walls of the patient’s uterus. When D&C or D&E is done due to miscarriages, abortions and retained products of conception, there’s a risk of developing Asherman’s syndrome.
Postpartum curettage: Here, curettage is performed due to complications such as retained placenta or postpartum haemorrhage.
Procedures of the uterus, like D&C for heavy bleeding and other uterine surgeries, are also risk factors.
Infections involving the uterus can include:
- Pelvic tuberculosis
- Pelvic infection post-delivery, abortion or miscarriage.
SYMPTOMS
Most of the symptoms of Asherman’s syndrome are related to the menstrual cycle or pregnancy. But it is possible that a patient suffering from Asherman’s syndrome may not show any symptoms at all.
Menstrual Cycle :
- Hypomenorrhea: In hypomenorrhea, the patient has highly light periods, i.e. reduced blood flow.
- Amenorrhea: The complete absence of menstrual periods is known as amenorrhea.
- Increased cramping during the menstrual cycle.
- Some patients may have no menstrual periods but still experience the pain associated with menstrual periods. This may indicate that menstruation is occurring, but the blood cannot exit the uterus due to blockage of the cervix by adhesions.
- If adhesions block the outflow of blood during the menstrual cycle, it can result in pelvic pain.
Pregnancy:
- Repeated miscarriages.
- Infertility
DIAGNOSIS
The following procedures are used to diagnose Asherman’s syndrome.
Hysteroscopy: Hysteroscopy is the gold standard for diagnosing Asherman’s syndrome. It is a procedure in which a small & lighted instrument known as a hysteroscope is inserted via the vaginal opening of the patient. This helps the doctor to have a look at the patient’s uterus. Most women do not require anaesthesia for this procedure.
Transvaginal ultrasound: In transvaginal ultrasound, the doctor inserts the ultrasound device 2-3 inches into the vaginal opening to ascertain the disorder. It is a painless procedure in which sound waves produce an image of the required organ.
Hysterosonogram: A hysterosonogram is a minimally invasive transvaginal procedure, also known as a saline infusion sonogram. It is similar to ultrasound, but in this procedure, the doctor also inserts a saline solution into the cavity of the uterus. This helps the doctor see things that would not be possible with normal ultrasound.
TREATMENTS
There are no medical studies that suggest that a particular treatment is better than others. Treatment basically involves removing the scar tissues and preventing them from growing again. Also, if the patient does not have any symptoms or the symptoms do not cause pain and obstruction in daily life, there is no medical reason why treatment should be pursued.
The treatment involves two stages:
1. Adhesiolysis (removal of the adhesions/scar tissue): This is the first step in treating Asherman’s disease; it is performed to remove the adhesions and is done using a hysteroscope. Adhesion removal can be difficult and must be done with care so that new scars are not created, further exacerbating the condition.
2. Preventing adhesions from growing again after adhesiolysis: One of the main challenges with treating Asherman’s syndrome is that it frequently returns even after the adhesion is removed. Results of adhesiolysis or surgical removal of adhesions may be good if the adhesions are mild to moderate with a high incidence of return of regular menses. Still, in cases of severe adhesions, a patient may require several repeated attempts of hysteroscopic surgery. Therefore, it is essential to prevent the adhesions from growing again. The following techniques may be used for the same:
Provision of oral estrogen: The patients can be given a course of estrogen to promote the growth of the normal uterine lining and prevent the growth of scar tissue again.
Placement of balloon or splint: A balloon-shaped IUD (intrauterine device) is placed to prevent the growth of adhesions again.